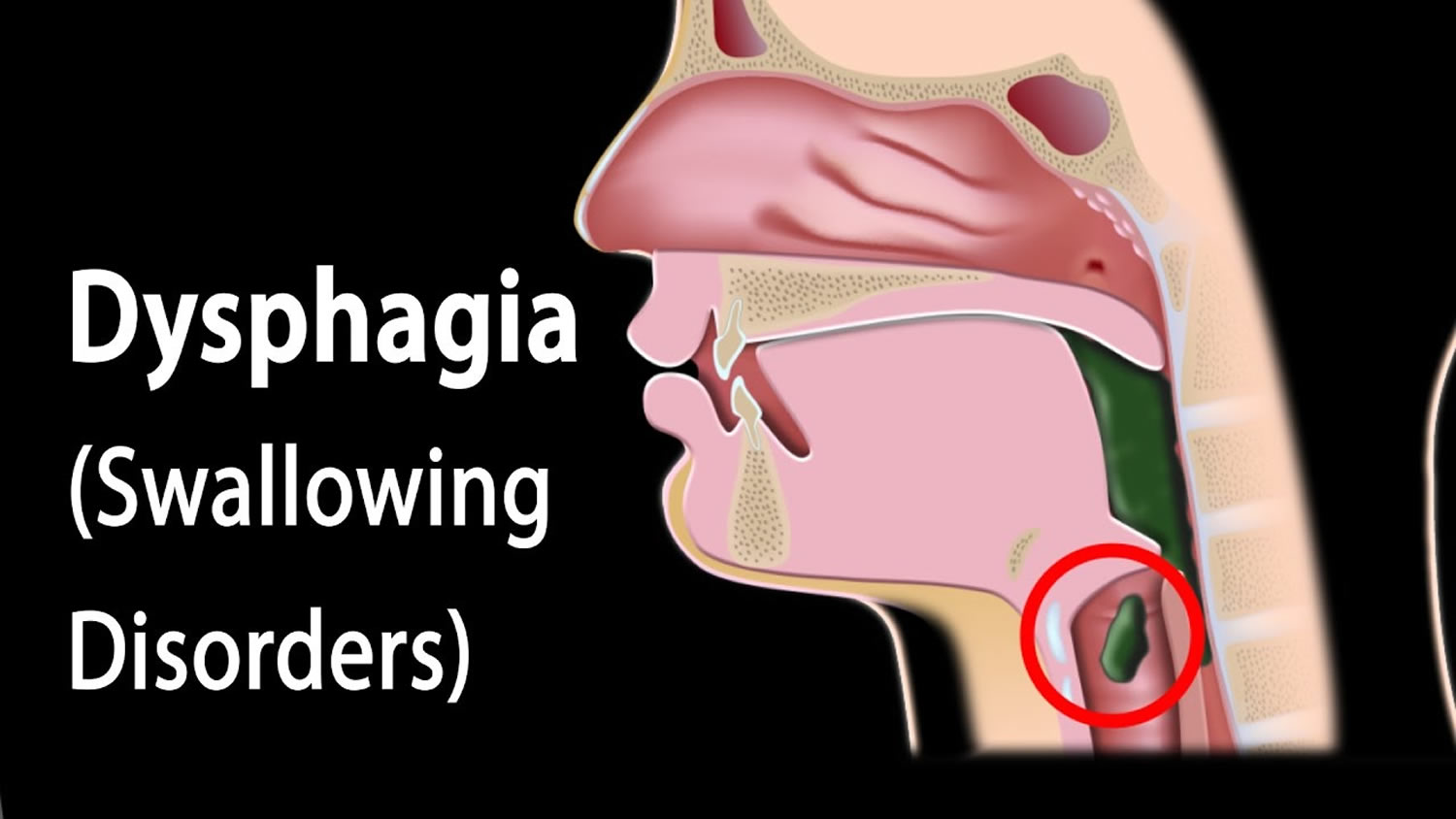
The word Dysphagia is from the Greek root “dys” meaning disorder and “phag” meaning food. People with dysphagia have difficulty swallowing and may even experience pain while swallowing (odynophagia). Some people may be completely unable to swallow or may have trouble safely swallowing liquids, foods, or saliva. When that happens, eating becomes a challenge. Often, dysphagia makes it difficult to take in enough calories and fluids to nourish the body and can lead to additional serious medical problems.
Course Objectives
Learn what dysphagia is and how it affects different populations
Learn how to treat dysphagia and minimize its effects
Understand dysphagia in the elderly, including those with dementia and Parkinson’s disease
Understand dysphagia’s connection to developmental disability
Learn techniques for handling youth dysphagia
Diabetes is a chronic health condition that affects how the body turns food into energy. When blood sugar goes up, it signals the pancreas to release insulin, which allows blood sugar into the body’s cells for use as energy. With diabetes, the body doesn’t make enough insulin or can’t use it as well as it should. Diabetes can cause serious health problems such as heart disease, vision loss, and kidney disease. This course is designed to familiarize students with the basics of diabetes and the ways that diet can affect the disease. Insulin resistance and diabetic metabolism are also comprehensively explained. Additionally, diabetes in the young, the elderly, and the developmentally disabled is covered in detail.
Course Objectives
Familiarity with the basics of diabetes
Comprehension of how diet affects diabetes
Understanding of insulin resistance and diabetic metabolism
Knowledge of diabetes management and treatment options
Awareness of the effects of diabetes on youth, elderly, and developmentally disabled populations
People vape with battery-operated devices used to inhale an aerosol, which can contain nicotine, marijuana, flavorings, and other chemicals. In many e-cigarettes, puffing activates the battery-powered heating device, which vaporizes the liquid in the cartridge or reservoir. The person then inhales the resulting aerosol or vapor. Research so far suggests that vaping is less harmful than combustible cigarettes when people who regularly smoke switch to them as a complete replacement, but e-cigarettes can still damage a person’s health. Vaping can lead to nicotine addiction and increased risk for addiction to other drugs. It also exposes the lungs to a variety of chemicals.
Course Objectives
Knowledge of what vaping is, how it works, and its physical effects
Familiarity with the risks involved with vaping
Insight into the teen vaping experience
Awareness of the connections between vaping and mental health issues
Overview of the effects of vaping in the disabled community
Understanding of the addiction experience and methods of quitting
Heat-related deaths and illnesses are preventable. Despite this fact, extreme heat kills approximately 1,220 people in the United States every year. Heat-related illnesses, like heat exhaustion or heat stroke, happen when the body is not able to properly cool itself. While the body normally cools itself by sweating, during extreme heat, this might not be enough. In these cases, a person’s body temperature rises faster than it can cool itself down. This can cause damage to the brain and other vital organs. Older adults, the very young, and people with mental illness and chronic diseases are at highest risk. However, even young and healthy people can be affected if they participate in strenuous physical activities during hot weather.
Course Objectives:
Obtain a fundamental understanding of heat risk and heat-related illness
Become familiar with methods of prevention and care
Learn the effects of excessive heat on children and the elderly
Know the risks of excessive heat for people with disabilities
Gain awareness of adverse heat effects on mental health
Understand the situations and needs of other high-risk groups
Cerebral palsy (CP) is a lifelong physical disability caused by a group of disorders that affect a person’s ability to move. The term “cerebral palsy” literally means that the brain lacks control over the muscles in the body. Damage to the developing brain during pregnancy or around the time of birth is the cause of CP. Body movement, muscle control, muscle coordination, muscle tone, reflex, posture, and balance are all affected by this disability.
This course offers a detailed description of cerebral palsy, including how it is diagnosed and classified. The types of CP vary widely, and each type is explained in full. Common treatments for CP are covered, along with the therapeutic approaches of music therapy and spider therapy. The course concludes with a discussion of the innovations made possible by artificial intelligence to improve the quality of life for people with cerebral palsy.
Course Summary
The Home and Community-Based Services (HCBS) Final Rule ensures individuals have full access to the benefits of community living and the opportunity to receive services in the most integrated setting appropriate. The purpose of the rules is to ensure that individuals receive services in settings that are integrated with and support full access to the greater community. This includes opportunities to seek employment and work in competitive and integrated settings, engage in community life, control personal resources, and receive services to the same degree as individuals who do not receive regional center services.
The Home and Community-Based Services (HCBS) rules enacted in 2013 ensure that people with disabilities have full access to and enjoy the benefits of community living through long-term services and support in the most integrated settings of their choosing. The thrust of this online course is for providers to understand what HCBS looks like in everyday life. The course does not cover the many deadlines and compliance mandates. The written and video content are as timely now as when this course was first created.
Course Objectives
Gain knowledge of the HCBS requirements and best practices
Steps to becoming HCBS compliant
Gain knowledge of the special HCBS rules as the rules apply to residential settings.
Taking this course again? Click this button.
Course Summary
PIN 22-13-ASC updates existing infection control prevention standards in community care facilities. COVID spread has heightened awareness in the disability community for more specific and compelling protocols to stop the spread of infectious diseases. Administrators will learn all aspects of infection control, from hand hygiene to creating a designated infection preventionist. Administrators can use the course content to develop infection control policies and training programs.
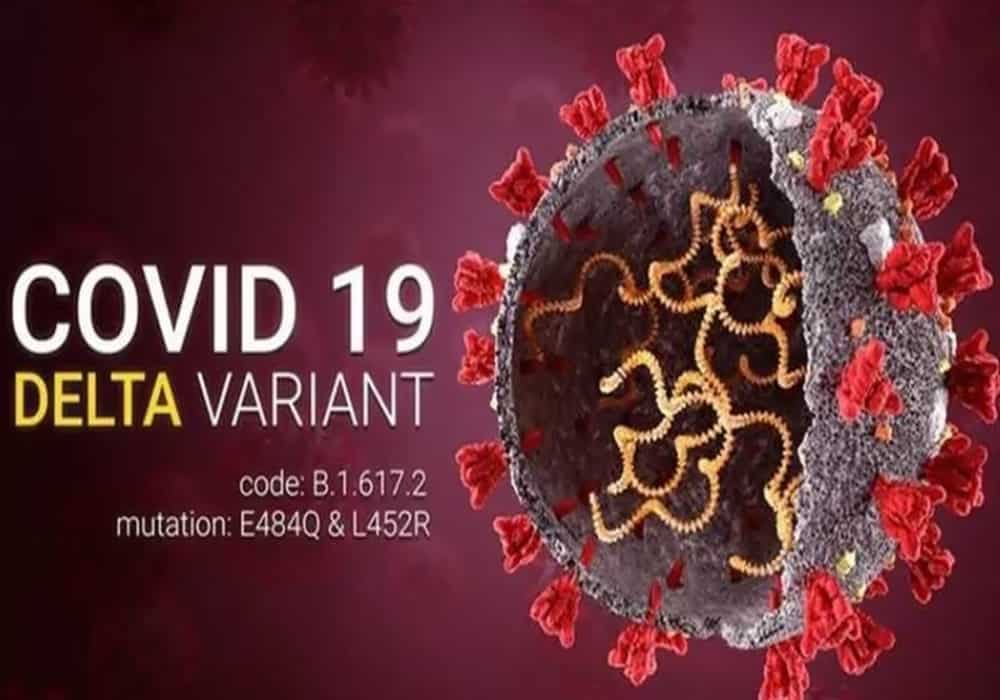
As more transmissible variants of COVID-19 have appeared, the study and understanding of Delta, Omicron, and further mutations have been of great importance in the fight against the virus. This course will cover COVID variants including Delta and Omicron in depth. The course will also discuss the benefits of vaccination and booster doses, as well as the potential problems associated with the lifting and loosening of restrictions. An overview of where we are today, including therapeutics and specialized boosters, will round out the course.
Course Objectives
Knowledge and understanding of COVID-19 variant strains
Understanding of the benefits of vaccination and boosters
Awareness of the potential for Omicron-specific boosters
Recognition of the effects of loosening and lifting restrictions
Awareness of the current situation regarding COVID and projections for the future

Taking this course again? Click this button.
Buildings and Ground section (80007) of Title 22 states that the facility shall be “clean, safe, sanitary and in good repair at all times for the safety and well-being of clients, employees and visitors. The licensee shall take measures to keep the facility free of flies and other insects.” Licensing requires a SIR to be filed if bed bugs are present in a residential facility.
Bed bugs are looking for a blood meal and may appear in any home at any time. Unfortunately, the presence of bed bugs in residential settings is a common problem. There is a general lack of knowledge re what bed bugs are, how to assess if they are present and how to eradicate them. Residents that are victims of bed bugs suffer from bites that leave ugly sores and possible infection. Ugly stains may appear on furniture and walls.
Bed bugs are tenacious creatures that often are hidden and difficult to find. No home is immune or safe from infestation. This online course will focus on to recognize an infestation, the health risks bed bugs pose, and how to prevent and eradicate them.
Course Objectives:
Know the facts about bed bugs and how they behave.
Learn methods of bed bug detection.
Understand the process of bed bug infestation.
Awareness of health risks associated with a bed bug infestation.
Familiarity with methods of bed bug prevention and eradication.
In-depth understanding of bed bug issues related to home health care.

Course Summary
According to the Centers for Disease Control and Prevention (CDC), falls are the leading cause of injury-related deaths for older adults. One in five falls causes serious injury such as a hip fractures or concussion. Problems with vision and balance, along with weakened bones and muscle loss, increase the risk for a fall.
Individuals with dementia are at higher risk for falls than people who do no have dementia. Impairment in judgment, sensory motor perception and difficulty communicating are a perfect storm for a fall. Individuals with dementia who do take a fall are at increased risk for serious fractures than elderly people who are not cognitively impaired. Many risk factors in the environment can be modified to prevent falls.
The course will also take a close look at how individuals with cerebral palsy are also at increased risk for falls.
Course Objectives:
Understanding of the prevalence and consequences of falls among the elderly
Knowledge of how dementia is associated with increased risk or falls.
Knowledge of how medication, vision and hearing issues, and orthostatic hypotension can increase the risk for falls.
Lean ways to alter the environment to prevent falls.
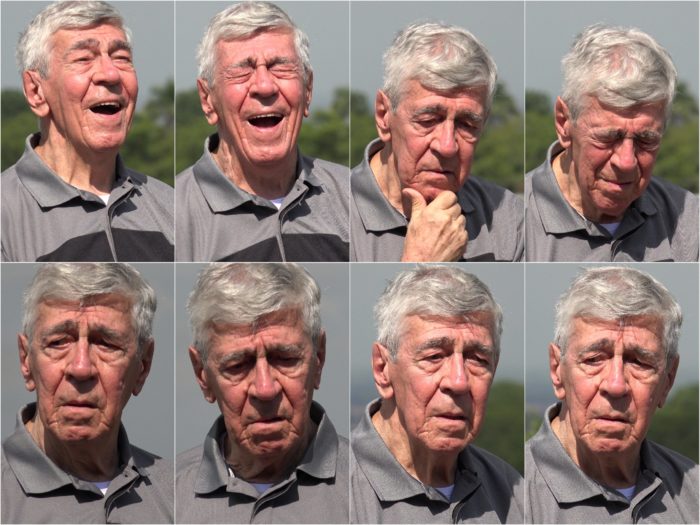
As the brain deteriorates in dementia, challenging behaviors often appear. These behaviors range from problematic to inappropriate to aggressive, and they can even be dangerous to the person with dementia and others involved. This course will take an in-depth look into behavioral issues related to dementia, their causes, and what can be done to manage them. Particular attention will be paid to empathic understanding of the reasons behind problem behaviors and the techniques involved in person-centered behavior management. Common behavioral problems such as wandering, rummaging, agitation, aggression, hallucination, delusion, and apathy will be covered in detail, illustrating the full range of behavioral problems likely to be encountered in Alzheimer’s and other forms of dementia.
Course Objectives
Understand how deterioration of the brain can lead to problems with behavior
Become familiar with the types of behavior issues associated with dementia
Understand the reasons that cause behavior issues
Know the difference between actual and perceived behavioral problems
Learn how to best manage difficult behaviors
Gain familiarity with person-centered behavior management
Learn the difference between behavior excesses and behavior deficits, and how to manage them